Easley Chiropractic for Post-Surgery Back Pain
Consideration: What is the incidence of individuals who have spine surgery and have partial relief, total relief, no change, or worsening of their pain?
- Considerations Before Choosing Surgery
- Outcomes and Costs of Back Pain Relief Options: Surgery and others
- Types of Back Surgery: Outcomes of Chiropractic for Back Pain
- Organized Medicine Recommends Spinal Manipulation for Back Pain
- Cox Technic for Back Pain Relief: Outcomes
- Why Chiropractic isn't as well used
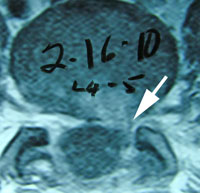
- Case Report: Cervical Spine Post-Surgery
- Case Report: Lumbar Spine Post-Surgery
- Closing Comments
- References
- 400 patients with sciatica resulting from a lumbar disc herniation were treated surgically or non-surgically. They were followed over a 10 year period and their clinical outcomes were compared. At 10 years post-surgery,
- 25% of surgical patients had undergone at least one additional lumbar spine operation.
- 25% of non-surgical patients had at least one lumbar spine surgery.
- 69% of surgically treated patients and 61% of non-surgically treated patients reported improvement in their predominant symptom of back or leg pain. (2)
-
Stenosis Surgical Vs. Non-Surgical Care Statistics: Again No Difference
- 97 patients with low back and leg pain due to spinal stenosis were treated surgically or non-surgically. At 8 to 10 years post-surgery,
- 53% of surgically treated and 50% of non-surgically treated patients reported that their predominant symptom of low back pain was improved.
- Both groups were satisfied with their current status:
- 55% of surgically
- 49% of non-surgically treated patients. (3)
Worker’s Compensation outcomes of single or multiple spine surgeries is not encouraging. Note:
- 600 single-operated workers compensation low back patients showed
- 71% did not return to work 4 years later
-
- 400 multiple-operated backs showed
- 95% did not return to work 4 years later (4)
-
- Cost of chiropractic care for the treatment of lumbar intervertebral disc herniation patients is 2% of total spent.
- A trial of conservative non-operative/non-surgical care is advised before surgery in patients with lumbar disc herniation.
- 30,709 patients with lumbar disc herniation cost a total of $105,799,925.
- During the 90 days before spine surgery, there was an average of $3,445 per patient spent.
- Average charge for discectomy procedure was $7,841.
- Charges:
- injection procedures totaled $16,211,246 or 32% of total charges
- diagnostic imaging $15,648,769 (31%)
- outpatient visits $6,552,135 (13%)
- physical therapy visits $5,723,644 (11%)
- chiropractic manipulation $1,177,406 (2%)
- preoperative studies $426,976 (0.8%)
- medications $263,039 (0.5%)
- miscellaneous charges $1,177,371 (2%) (5)
-
- from 1.3 to 19.9 per 100, 000 beneficiaries.
Life-threatening complications increased with increasing surgical invasiveness:
- from 2.3% among patients having decompression alone to 5.6% among those having complex fusions.
Adjusted mean hospital charges were high:
- for complex fusion procedures $80,888 compared with $23,724 for decompression alone. (6)
Boyle reported in Fortune Magazine on the cost and incidence of low back pain in the United States that:
- Back pain is the 2nd most common reason to see a doctor.
- The World Health Organization says low back pain is an official epidemic.
- Duke University reports that
- 26 billion dollars is spent a year on back care and
- 10% of back patients with chronic low back pain absorb 90% of the cost
-
- Orthopedic surgeons and chiropractors make up the standard approach to treatment.
- 1,175,000 in-patient spine surgeries were performed last year
- Back surgery is big business - $40,000 for fusion
- 22% growth in implants and devices
- James Weinstein, MD, Chief Of Orthopaedic Surgery, Dartmouth Medical School, Editor, Spine, is the source of this information. (7)
Consider the following facts on surgical interventions for spine care in the United States and cost and outcomes of this modality: (8)
- New surgical implant devices increase lumbar fusion rates dramatically in medicare patients in 306 us hospital
- 20-fold in surgical rates among medicare enrollees from 1992-3 to 2002 and 03 in lumbar fusion.
- This represents the largest coefficient of variation seen with any surgical procedure. Medicare spending for inpatient back surgery more than doubled over the decade.
- Spending for lumbar fusion increased more than 500%, from $75 million to $482 million.
- 1992 - lumbar fusion represented 14% of total spending for back surgery
- 2003 - lumbar fusion accounted for 47% of spending for back surgery.
-
- Dr. Cox notes: Williams reported that chiropractic care is 2.9 % of the cost of back care. How does this continue?
Washington State Worker’s Compensation data from 1994 to 2001 compared lumbar fusion with cages and instrumentation to non-surgical care in 1950 subjects.
- Lumbar cage fusion rates increased from 3.6% in 1996 to 58% in 2001: result was increased complication risk without improving disability or reoperation rates.
- 2 years after fusion
- 64% disabled
- 22% re-operation
- other complications 12%
-
- Lumbar fusion devices compared with exercise and cognitive intervention are no better in randomized control trials (RCTs).
- Use of cages or instrumentation was associated with increased complication risk compared with bone-only fusions without improving disability or reoperation rates.
Use of intervertebral fusion devices rose rapidly after their introduction in 1996. This increased use was associated with an increased complication risk without improving disability or reoperation rates. (9)
Comparison Of Spinal Surgery To Intensive Rehabilitation For Patients With Chronic Low Back Pain Shows Equal Outcome.
349 chronic low back patients aged 18-55 years old were studied to compare surgical stabilization with intense rehabilitation. It was found that there is no evidence that surgery was any more beneficial than intensive rehabilitation. The authors concluded that surgery costs more with morepotential risk, and is not cost effective. (10)
Probably no area of chiropractic spinal manipulation is as challenged as treating the post-surgical patient who is the same, worse, or disenchanted with their surgical outcome. Certainly, the opportunity to treat the patient before surgical intervention is best. When confronted with this post-surgical patient, however, the chiropractic physician proceeds as if with a patient who has not had surgery. i.e. The chiropractor will proceed with the careful history and clinical examination to determine what is causing the pain. That cause may be within the surgical site or adjacent to it. In treating the post-surgical spine, fusion or no fusion is a dictator of care. If there is a fusion, spinal manipulation is given to adjacent levels of the spine to the fused area. If there is no fusion, the doctor carefully proceeds as if no surgery. Some motion may be possible within the spine depending on the surgical procedure performed. (11)
Let’s look at some factors of interest and importance to a patient seeking chiropractic care for their post-surgical spinal problem. (11)
Utilization of Chiropractic
The utilization of chiropractic Cox Flexion Distraction Decompression spinal manipulation is suitable with the direction of spine care in the United States today. Chiropractic patient visits increased dramatically with the total number of United States adults who visited a chiropractor increasing 57% from 7.7 million in 2000 to 12.1 million in 2003. From 1997 to 2006, the inflation-adjusted national expenditures on chiropractic care increased 56 percent from $3.8 billion to $5.9 billion. (11)
DC vs MD Outcomes: Cost, Workdays, Compensation Paid
In North Carolina, a study of utilization, treatment costs, lost workdays, and compensation paid workers with musculoskeletal injuries treated by medical doctors (mds) and doctors of chiropractic (DCs) were compared in a retrospective review of 96,627 claims. Average cost of treatment, hospitalization, and compensation payments, lost workdays, and cost of care was higher for patients treated by MDs than for patients treated by DCs. Despite the lower cost of chiropractic management, the use of chiropractic services in North Carolina appears very low. The average treatment cost for patients treated by MDs was $3519, whereas the average treatment for chiropractic patients was $663. Under the low back injury category, the average costs of care were $3425 for MDs and $634 for DCs. Compensation payment averaged $15,819 for patients treated by MDs, $1912 for patients treated by DCs, and $19,596 for patients treated by both. The average total cost of claims (including compensation) managed by MDs was $23,562; for claims managed by DCs it was $2597; and for combined care it was $29,446. (12)
Distraction Reverses Disc Degeneration
Discs have been seen to regenerate. Following 28 days of compression in rabbit discs which caused degeneration and then given 28 days of distraction applied, discs were seen to reverse their degenerative change with regenerative evidence. This was seen on mri study. Distraction results in disc rehydration, stimulated extracellular matrix gene expression, and increased numbers of cells. Disc distraction enhances hydration in the degenerated disc and may also improve disc nutrition via the endplates. (13)
Safety Of Cox Flexion Distraction Spinal Manipulation
The safety of Cox Flexion Distraction Protocols was compared to other forms of spinal manipulation. It showed almost no adverse side effects in its clinical application of manipulation to the doctor administering the treatment and 1 in 54 of patients being manipulated. The following chart shows the comparison of various techniques of spinal manipulation to Cox Flexion Distraction spinal manipulation. (14)
- Adjusting Technique injuries from adjusting / injuries from being adjusted
- Diversified 280 cases 61 74
- Thompson 142 cases 3 25
- Gonstead 135 cases 31 39
- Cox F/D 54 cases 0 1
Radicular lumbar spinal stenosis patients over 70 with radicular symptoms are good candidates for conservative treatment as long as complete myelographic block is not present. (15)
Organized medicine recommends spinal manipulation for the treatment of back pain. See the following statistics and facts:
- Spinal manipulation is recommended by the American Pain Society and the American College of Physicians for primary care of low back pain.
- Prolotherapy, facet joint injection, intradiscal steroid injection, and percutaneous intradiscal radiofrequency thermocoagulation are not effective.
- Epidural steroid injections give short term but not long term relief of pain.
- Spinal cord stimulation is moderately effective for failed back surgery syndrome with persistent radiculopathy, though device-related complications are common.
- Surgery for leg pain (radiculopathy) with herniated lumbar disc and symptomatic spinal stenosis is associated with short-term benefits compared to nonsurgical therapy, though benefits diminish with long-term follow-up.
- For patients with no leg pain (nonradicular back pain) with disc degeneration, fusion is no more effective than intensive rehabilitation, but associated with small to moderate benefits compared to standard nonsurgical therapy. (18)
Low back pain is divided into three types: non-specific low back pain, back pain with radiculopathy or spinal stenosis, back pain with other specific causes. Spinal manipulation, acupuncture, exercise, massage, yoga are recommended for treating low back pain. (19)
In a classic determinative study of who patients with low back pain seek care from, 33% of 27,810 people chose chiropractors as their treating physician for low back pain in the national health and nutrition examination survey (nhane) (20) In the United States, spine care is delivered 60% by the medical model and 40% by the chiropractic model. (21)
A randomized clinical trial study comparing Cox Flexion Distraction spinal manipulation to medical care for chronic low back pain showed flexion distraction gave superior outcome. (22)
The benefits of Cox Flexion Distraction And Decompression spinal manipulation was compared to medical care in 235 patients who were randomized to cox flexion distraction spinal manipulation to medical care. The outcome showed
- flexion distraction treated patients had significantly greater relief from pain
- patients with radiculopathy did significantly better with flexion distraction than medical care
Long term followup of patient relief of low back and leg pain comparing Cox flexion distraction spinal manipulation to medical care showed less recurrence of pain with Cox spinal manipulation compared to physical therapy.
- 38% of flexion – distraction patients and 54% of physical therapy patients sought care for low back pain during the follow-up of one year.
- Physical therapy subjects attended significantly more health care visits than those receiving chiropractic care. (23)
Long term follow-up of patient relief of low back and leg pain comparing Cox Flexion Distraction spinal manipulation to medical care showed greater relief of pain for 1 year with Cox spinal manipulation compared to physical therapy.
Flexion distraction chiropractic manipulation was found more effective in reducing pain for 1 year when compared to a form of physical therapy. (24)
Flexion distraction spinal manipulation was given to 49 consecutive patients with disc herniation confirmed on MRI with pain and disability for an average of 60.5 weeks, 2-3 times a week initially for 3 weeks. The clinical outcomes at the end of treatment and at 14.5 months later were clinically meaningful.
- At end of treatment:
- Improvement of pain in 79%
- Improvement of disability in 70%
-
- At 14.5 months later:
- Improvement of pain in 79%
- Improvement of disability in 73 (25)
-
Consider the following facts on spinal stenosis of the lumbar spine with the clinical help of flexion distraction spine manipulation for it:
- Lumbar spinal stenosis patients improved by 76% and disability improved in 73% in 57 patients treated with Cox distraction and/or neural mobilization. (26)
- The cost of treating back pain is tremendous with 5% of the patients absorbing 75% of the cost which exceeds 100 billion dollars a year. (27)
Why aren't these new concepts of chiropractic treatment more widely known and practiced? Because of the following documentation:
- quote from National Academy Of Sciences: "An average of about 17 years is required for new knowledge generated by randomized clinical trials to be incorporated into practice, and even then application is highly uneven…and there are insufficient tools and incentives to promote rapid adoption of best practices.” (28)
Examples Of Surgical Cases With Increased Symptoms And Pain Afterwards




In looking at the surgical cases above, one wonders what the surgical success rate is. In a study to determine surgical success rates, the total increased satisfaction was 40%, re-herniation rate was 9% and return to work frequency was 64% for both one level open discectomy and microdiscectomy. (29) One consideration of "surgical success" is the activity of the patient before and after surgery. Woolcott (30) showed that among those over age 65 years, physical activity is strongly associated with reduced health resource use and costs. Therefore, it is important to get back into your activities of daily living so as to rebuild your general back and general health to avoid future spine pain after getting a handle on post-surgery pain. Don't let pain stop you.
Contact Young Chiropractic for an evaluation and treatment plan to help you regain your quality of life after back surgery.
